What can an ENT do via an online or telemedical or telehealth visit?
While everyone understands the utility of seeing a psychiatrist or a primary care physician via video chat, it can be hard to see how a specialist visit can be done online. Still, my experience and the available evidence suggests it can be really helpful. Additionally, currently during the coronavirus pandemic, the American Academy of Otolaryngology Head and Neck Surgery is recommending all providers limit patient care to urgent and emergent in-person visits.
To begin, I would argue that most of the diagnosis for any medical specialty comes from the doctor actively listening to the patient’s story and symptoms and asking poignant questions.
Furthermore, most experienced physicians have a sort of ‘spider sense’ about who is sick and worrisome, and whose symptoms can be monitored for a bit longer. Video chat allows us to determine this by actually seeing the patient face-to-face.
In ENT, through the use of video, we can examine a lot of the facial anatomy.
Things we can do:
-a decent cranial nerve exam
-evaluate any swelling or skin lesions
-check eye/neck/tongue/facial muscle movements
-assess bleeding
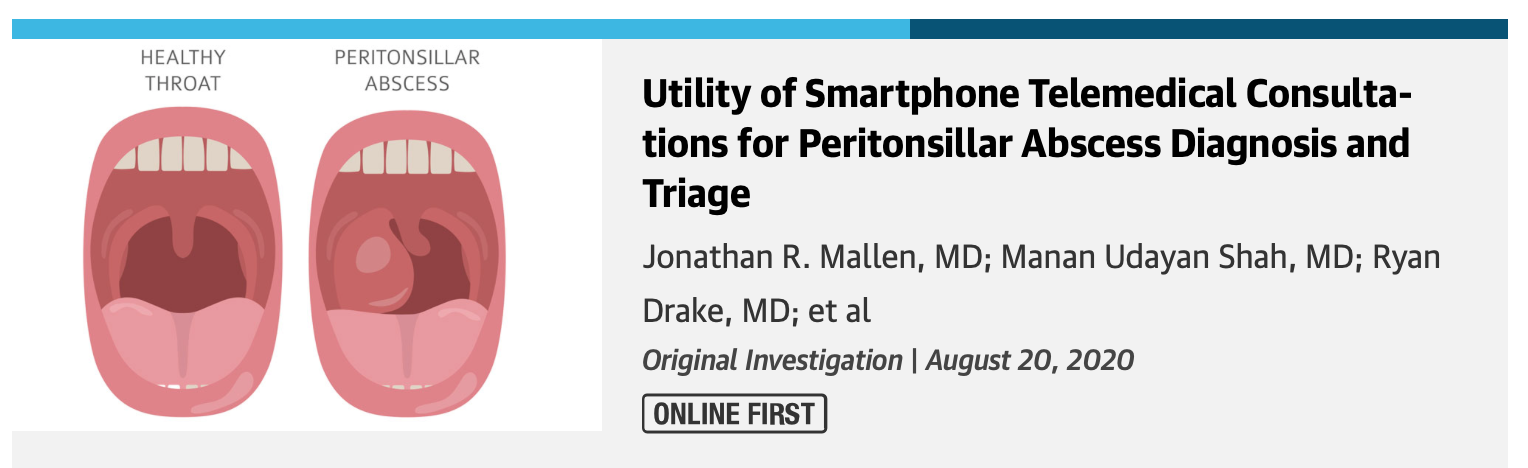
-with the use of a camera flash or flashlight, you can actually get a decent oral cavity exam

(This isn’t as good as an exam with a tongue blade, but it certainly allows visualization!)
-with some software, the patient or a family member can even transmit an ear exam of anterior nose exam if they purchase a device like the firefly otoscope
Together, all of this information can provide an ENT with a good sense of how to begin treating a patient. More importantly, it can help an ENT to determine whether a patient needs to be seen in the office or not.
What can’t be done online? (Why an ENT may ultimately want to schedule an in-person visit)
The beauty of online visits is that it helps to determine who may need to be seen in-person at an office.
For some symptoms, we will need to perform a hands-on exam at our office to ensure we are not missing anything concerning (like an infection or cancer).
Often, your doctor may want to use a microscope or endoscope to examine a patient more closely. We call this ‘endoscopy,’ and it is typically quick and pain-free. It allows us to examine internal regions of the body or regions of the body that cannot be adequately observed with the naked eye. When making certain diagnoses, this type of in-person observation can provide vital information.
I have included some endoscopy images below to give a sense of how much detail and anatomy we can observe with a physical exam in the office.
(Above: on the viewers left a normal eardrum, on the viewers right a septal spur in the nose)
Should a patient be seen online or in person? The beauty is a patient doesn’t necessarily need to decide. Many ENTs are now offering online visits as a screening method. Depending on the results of your online or telehealth visit, your doctor may or may not ask you to come into the office.
39.644161
-104.916652